Wilson’s Disease – All you need to know
Wilson’s disease is a rare genetic syndrome in which the liver, brain, and other vital organs accumulate copper. Wilson’s syndrome is most common in children between the ages of five and thirty-five. Continue reading to learn more.
Wilson’s disease is a rare genetic condition in which copper builds up in the liver, brain, and other essential organs. Wilson’s disease most often occurs between the ages of 5 and 35. However, it can also affect younger and older adults.
There are people in Mumbai who suffer from the disease mainly due to their genetic issues. A patient with Wilson’s disease can lead a quality life by availing of proper treatment from a liver transplant surgeon in Mumbai.
Copper is essential for developing healthy nerves, muscles, collagen, and the skin’s pigment melanin. Generally, our body absorbs copper from the food we eat and exerts the excess through bile secretion.
On the other hand, the excess copper accumulates in the body of people with Wilson’s disease. This high level of copper accumulation is very harmful to your health. Wilson’s disease is treatable if identified early, and even individuals with this condition lead normal lives.
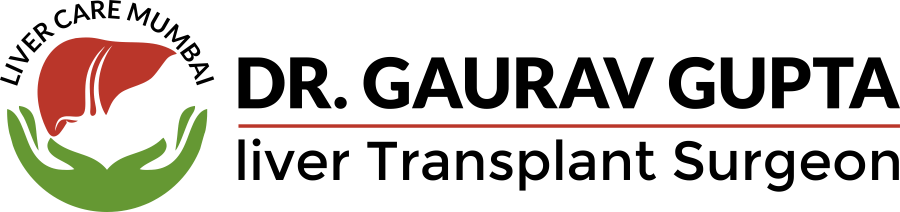
What are the symptoms of Wilson’s disease?
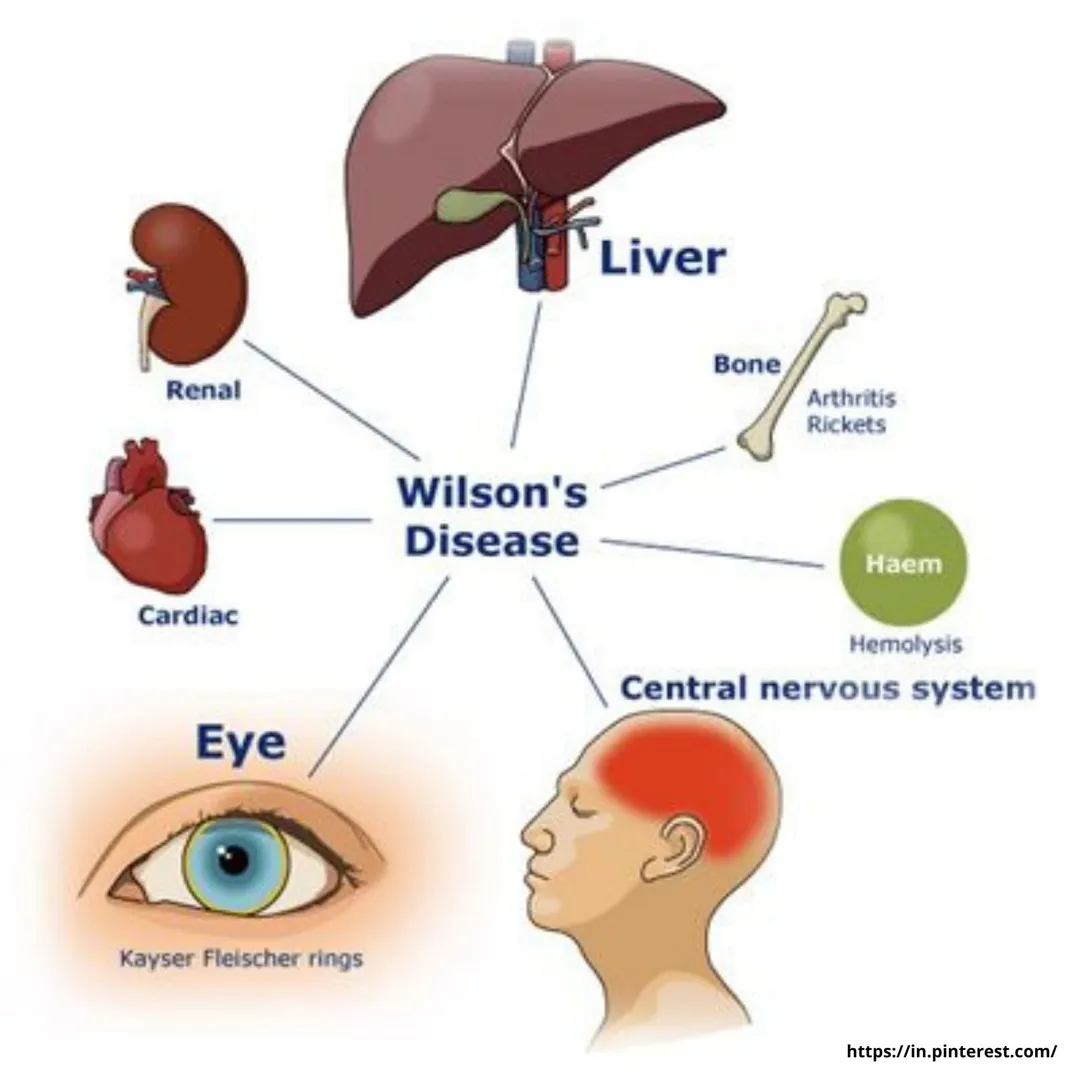
Wilson’s disease occurs by birth, but symptoms do not occur until copper levels in the brain, liver, or other organs have increased. The signs and symptoms of the disease differ based on the affected body parts. They may contain the following:
- Fatigue, a loss of appetite, or stomach pains
- Jaundice
- Discoloration of the eyes (Kayser-Fleischer rings)
- In the legs or lungs, there is a build-up of body fluid.
- Issues while talking, chewing, or physical coordinating
- Muscle tightness or uncontrollable motions
If a person experiences any of the mentioned symptoms, he or she should avail liver transplant after having a consultation.
How does Wilson’s disease happen?
Wilson’s disease is hereditary. It is an autosomal recessive disorder, which means the patient must inherit one problematic gene from each parent. The person won’t get sick if you get one rare gene, but you will be a vector and pass the gene on to your offspring.
The cases of Wilson’s disease in India are increasing and many liver surgeons observe patients complaining about this condition. More and more awareness needs to be made so that early diagnosis is possible for Wilson’s patients.
How does a liver transplant doctor diagnose Wilson’s disease?
Wilson’s disease is challenging to diagnose, and its signs and symptoms are also difficult to distinguish from those of other liver disorders, like hepatitis. The diagnoses are based on the symptoms and tests. These include:
- Tests of the blood and urine: Blood tests are essential to evaluate your liver function. It helps to check the level of ceruloplasmin, a protein that binds copper in the blood and copper in the blood. The doctor will also want to monitor the amount of copper excreted in your urine over a day.
- Eye examination: An ophthalmologist tests Kayser-Fleischer circles’ eyes. Excess copper causes complications in the eyes. Wilson’s disease is also related to a cataract form known as a sunflower cataract, which can come out during an eye test.
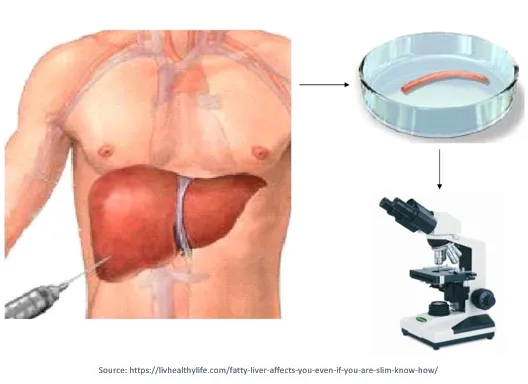
- Biopsy: A thin needle is inserted through your skin into your liver, where we take a small tissue sample. Then the tissue goes for examination in a laboratory to check the excess copper.
- Genetic testing: If Wilson’s disease occurs due to genetic abnormalities, genetic testing will detect that from the patient’s blood sample. Knowing the family’s mutations helps doctors to test siblings and start treating them before signs occur.
Now let us see the treatment for Wilson’s disease
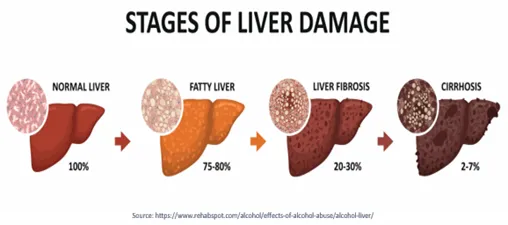
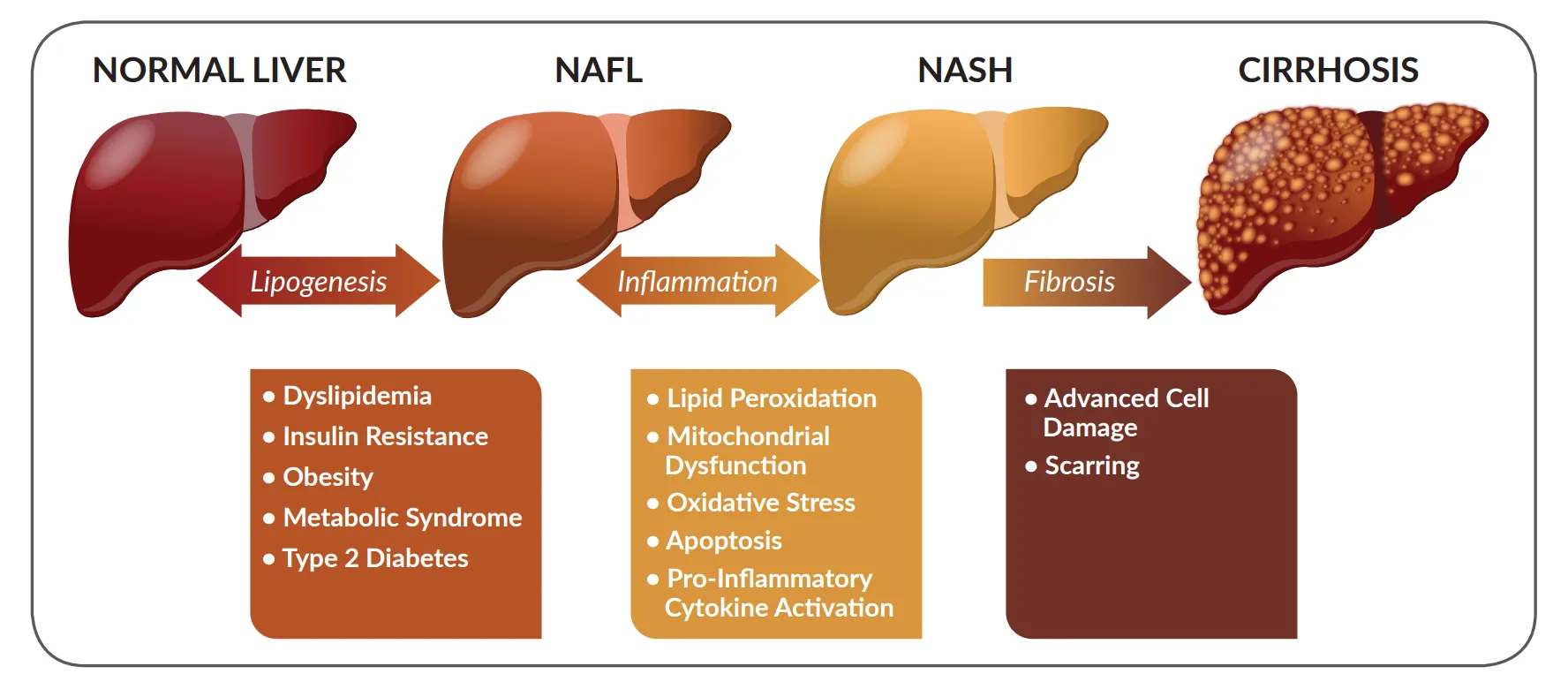
The doctor may prescribe proper medications to bind copper and then release them into the bloodstream. Finally, they will be released through your urine. After that, the treatment stops the copper formation. The doctor may also suggest a liver transplant if there is serious damage to the liver.
Prescription drugs
If a patient has Wilson’s disease, they will have to take drugs for the rest of your life. The medications include the following:
Note: Below drugs can be taken only on the prescription of a qualified doctor. Self-diagnosis can land a patient in trouble.
- Penicillamine: It is a chelating agent that may have severe side effects, including skin and renal disorders, bone marrow suppression, and deteriorating neurological symptoms. If a person is allergic to penicillin, he or she will require proper supporting remedies for allergy. You will need to take vitamin B6 supplements in limited doses.
- Triennial: Trientine is similar to penicillamine, but it has fewer side effects. However, it can escalate few neurological problems also.
- Galzin: Galzin drug prevents the body from consuming copper from food. It may bring stomach disturbance.
Surgical techniques
A patient may require a liver transplant if the liver damage is severe. The liver transplant removes the diseased liver and replaces it with a healthy liver from a donor during a liver transplant.
Are there any home treatments/remedies available for Wilson’s disease?
If a person has Wilson’s disease, the doctor would typically encourage limiting the copper intake from a regular diet. Even the person should avoid copper-containing multivitamins.
Avoid food items like mushrooms, chocolate, shellfish, liver, or any other copper-rich food. Further diet control can be prescribed only after proper diagnosis of the patient
Frequently Asked Questions :
1. How long can you live with Wilson disease?
Life expectancy without treatment is expected to be 40 years, although patients who receive quick and effective treatment may live a normal lifespan.
2. Is Wilson’s disease reversible?
Wilson disease has no known treatment. Copper-chelating drugs, which help your body’s organs and tissues get rid of excess copper, are one type of treatment that may be required for the rest of your life.
3. Who is most likely to get Wilson’s disease?
Wilson disease is more common in people under the age of 40. By the age of four, children begin to display symptoms. The organs that are impacted, stop functioning normally. Eastern Europeans, Sicilians and southern Italians are the most affected, but it can affect anyone.