Alcoholic liver disease results from overconsumption of alcohol. It leads to liver damage, causing fat build-up, inflammation, and scarring of the liver. It can affect the whole body and can be fatal. The first and foremost step after diagnosis of alcoholic liver disease is consulting a liver specialist.
Dr. Gaurav Gupta, an experienced liver specialist in Mumbai, provides effective alcoholic liver disease treatment in Mumbai. Presently, he is a Consultant and HOD of the Liver Transplant and HPB Surgery at Fortis Hospitals, Mulund, Mumbai.
Dr. Gupta is well-known for his expertise in the field of Liver Transplant. He has conducted 500+ liver transplants. Furthermore, Dr. Gupta has 15+ years of surgical experience, out of which more than ten years in Liver Transplantation.
Overview of alcoholic liver disease, its stages, symptoms, diagnosis, and alcoholic liver disease treatment.
What is Alcoholic Liver Disease?
Excessive alcohol consumption causes alcohol-related liver disease. It’s a widespread liver disease that can be prevented at an initial stage. Alcohol abuse causes injury to the liver as the alcohol metabolizes in the liver.
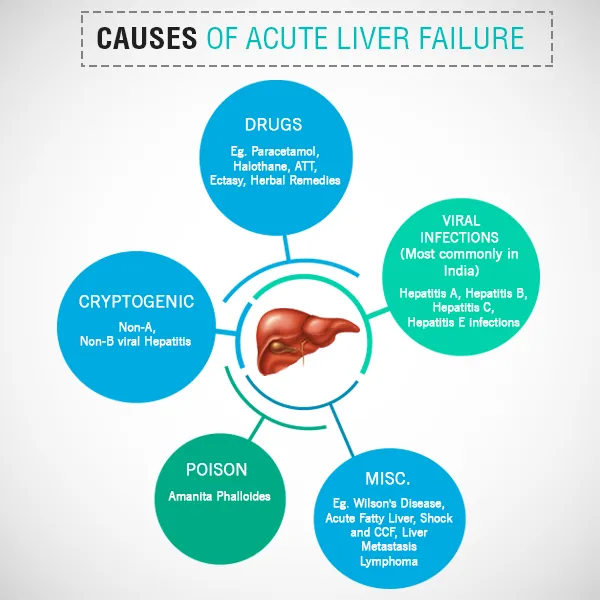
Liver specialists advise patients with alcoholic liver disease to take a preventive vaccination for Hepatitis A and Hepatitis B.
Stages of Alcohol-Related Liver Disease and Associated Symptoms
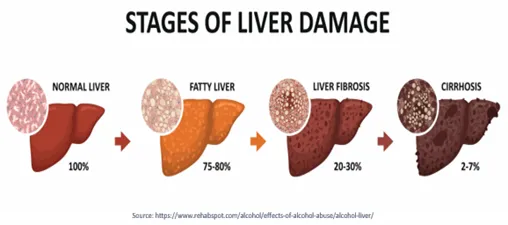
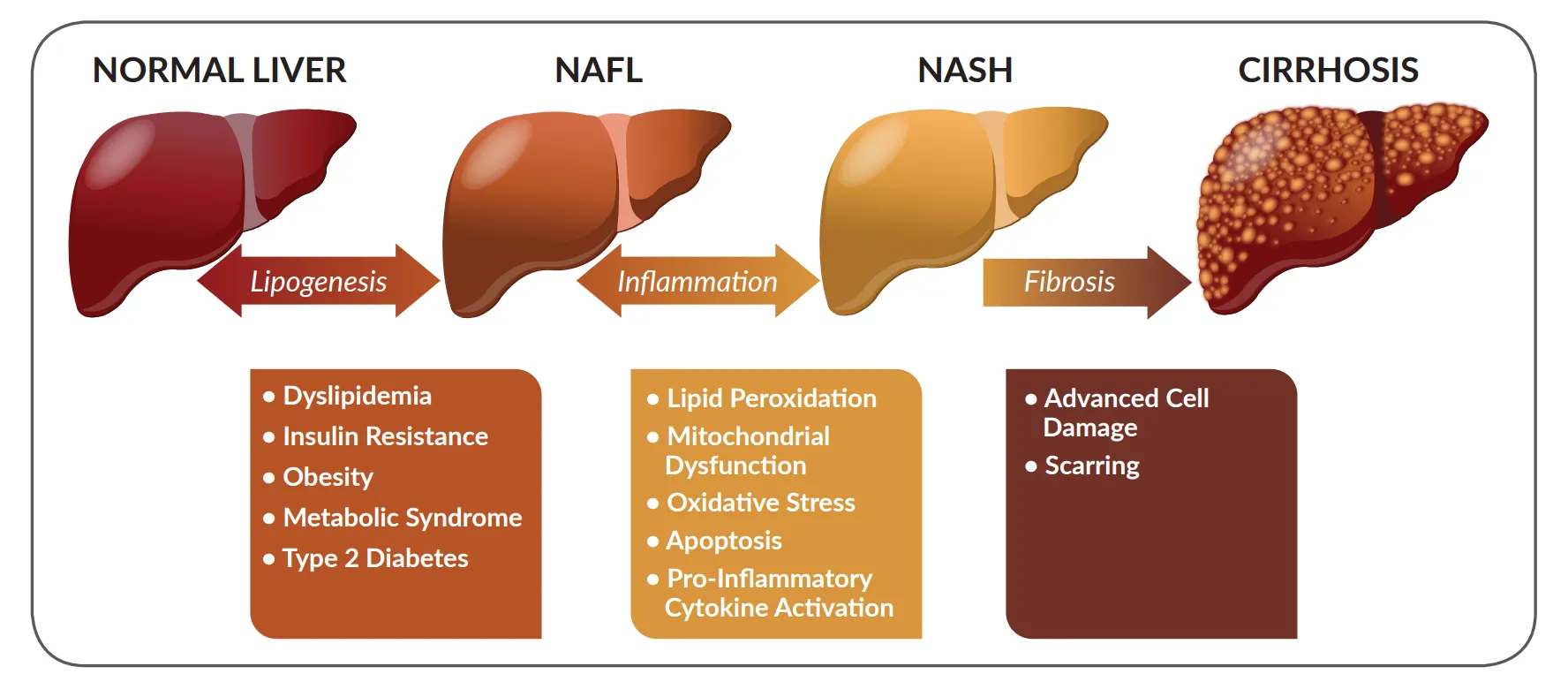
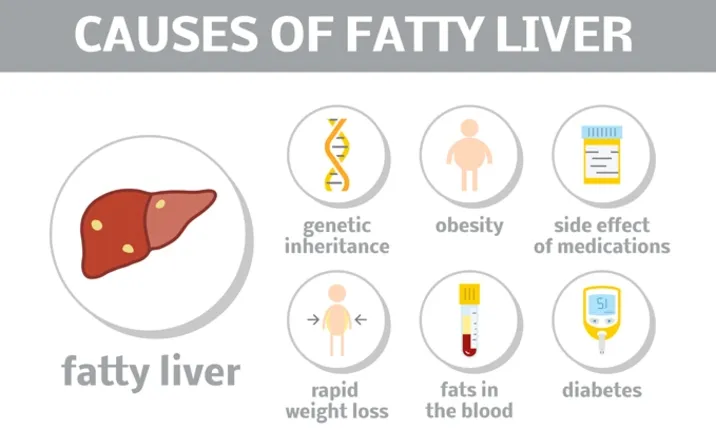
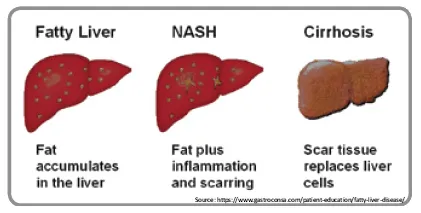
Stage I: Fatty liver
Fatty liver is an excessive accumulation of fats inside the liver cells. It is a common alcohol-related liver disorder. The liver enlarges, causing upper abdominal discomfort on the right side.
Stage II: Alcoholic hepatitis
Alcoholic hepatitis is liver inflammation that causes the destruction of liver cells as well as scarring. Fever, jaundice, an elevated white blood cell count, a rise in liver enzymes ( SGOT and SGPT) a swollen, tender liver, are all possible symptoms.
Stage III: Alcoholic cirrhosis
Alcoholic cirrhosis causes the loss of normal liver tissue and the formation of non-functioning scar tissue. Alcoholic hepatitis if left unchecked leads to permanent scarring and irreversible damage to the liver which is called cirrhosis. In this stage liver changes to a hard, nodular irregular surface and small in size. Symptoms may include portal hypertension (blood vomiting), enlarged spleen ascites, heavy bleeding (due to poor clotting), kidney failure, confusion, and liver cancer.
How is Alcoholic Liver Disease diagnosed?
- Alcoholism history:
Drinking over 20 units of alcohol a week (one unit equals one bottle of beer or a peg of whisky or a glass of wine) for more than ten years.
- Liver function tests:
A series of blood tests is used to see whether the liver is working correctly.
- Imaging tests:
CT scans or ultrasounds to view the structural anomalies of the liver.
- Fibroscan:
Fibroscan tells us about liver damage. It let us know if fibrosis has started in the liver which will suggest advanced alcoholic liver disease.
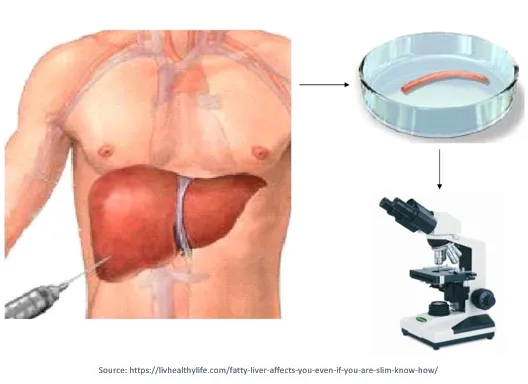
A process in which liver tissue samples are examined under a microscope to diagnose any underlying conditions. These days use of liver biopsy is very limited in diagnosing Liver disease.
Alcoholic Liver Disease Treatment in Mumbai
A liver specialist initiates specific treatment for the alcohol-related liver disease based on the disease’s stage and the patient’s acceptance to quit alcohol. Treatment aims to recover some or all of the liver’s normal functions.
In Stage I: The first step of treatment for fatty liver and early stages of alcoholic hepatitis is avoiding alcohol.
- Alcohol Cessation
If a person has alcoholic hepatitis, the only way to recover is to stop drinking alcohol. It will help reverse the liver’s damage and prevent it from worsening. If the patient is heavily dependent on alcohol and wants to quit, there are many options available. Medication, counseling, community groups, and a residential treatment facility are some of the alternatives.
- Treatment for Malnutrition
If the patient has appetite loss, the doctor can suggest a special diet to balance nutrients and vitamins. In extreme situations, tube feeding is also advised. A high protein and high-calorie diet help in recovering from alcoholic liver disease.
- Medication to Reduce Liver Inflammation
If the patient has severe alcoholic hepatitis, the liver specialist can prescribe corticosteroids and pentoxifylline to decrease liver inflammation.
In Stage II, simply abstaining from alcohol should be enough to regulate and even cure the problem. The liver is a potent healer. It can also restore some of the damage caused by alcohol. Cirrhosis scarring, though, is the only condition it can’t repair.
In Stage III, after the progression of cirrhosis, the disease will eventually worsen. With alcohol abstinence, however, the pace of improvement is substantially slowed. When advanced cirrhosis sets in, the only treatment is total abstinence from alcohol and liver transplantation. Once there are Liver cirrhosis complications, unfortunately, medication will not be able to cure the problem and the only long-term solution remains a liver transplant.
Book an appointment with Dr. Gaurav Gupta to avail of the most effective alcoholic liver disease treatment in Mumbai.
Frequently Asked Questions:
Q. Is Alcoholic Hepatitis More Prevalent In Men Or Women?
Women tend to be more susceptible to alcohol-related liver injury. Even if a man and a woman have relative weight and consume the same amount, the woman’s blood-alcohol level is higher than the man’s due to her more body fat and lower water content.
Q. Is It True That All Alcoholics Develop Alcoholic Hepatitis And Cirrhosis?
No, it’s not true. Some alcoholics can experience extreme physical and psychological symptoms of alcoholism while preventing severe liver damage. Alcoholic cirrhosis affects between 10% to 25% of alcoholics.
Q. Does Alcoholic Hepatitis Always Develop Into Cirrhosis?
No, it’s not true. Cirrhosis typically takes several years to develop after alcoholic hepatitis has caused enough liver damage. Cirrhosis can be prevented if alcoholic hepatitis is detected and treated earlier.
Q. How Long Can One Live With Alcoholic Liver Disease?
Depends on the stage of liver disease. In the initial stages, abstinence from alcohol and proper treatment can cure the disease. Once Cirrhosis sets in then depending upon the stage of cirrhosis different complications can develop.
Q. Can Patients start alcohol after Liver Transplant?
Strictly No. Once patients undergo Liver transplants they are advised to abstain from alcohol for life long.